What is Nephrology and What Does a Nephrologist Do?
Nephrology is a specialty of Internal Medicine that focuses on the treatment of diseases that affect the kidneys.
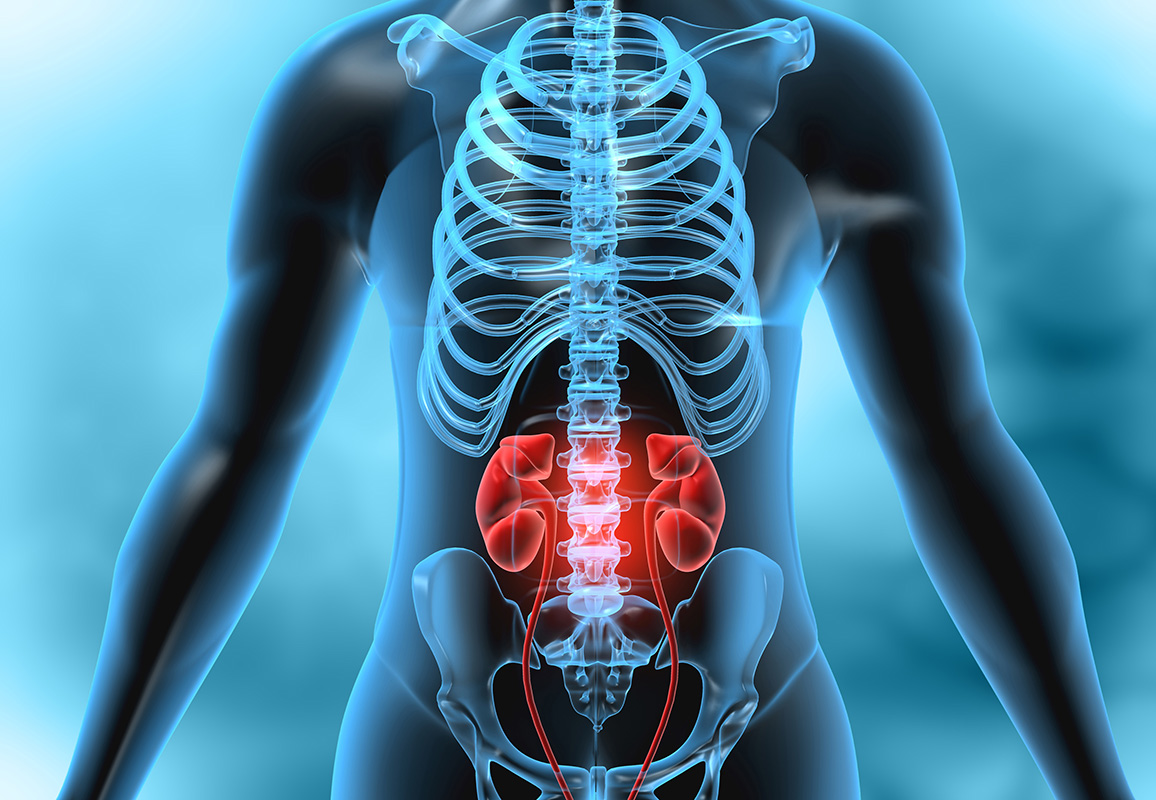
Your kidneys are located below your ribcage on either side of your spine. They have several vital functions, including:
- removing waste and excess fluid from the blood
- maintaining your body’s electrolyte balance
- releasing hormones with functions such as managing blood pressure
A Nephrologist’s Job
A Nephrologist is a physician that specializes in treating diseases of the kidney. Not only do Nephrologists have expertise on diseases that specifically affect the kidney, but they’re also very knowledgeable about how kidney disease or dysfunction can affect other parts of your body.
Although your primary care doctor will work to help prevent and treat early stages of kidney disease, a Nephrologist may be called in to help diagnose and treat more severe or complex kidney conditions.
Conditions a Nephrologist Treats
Nephrologists can work with you to help diagnose and treat the following conditions:
- Blood or Protein in Urine
- Chronic Kidney Disease
- Kidney Stones
- Kidney Infections
- Kidney Swelling Due to Glomerulonephritis or Interstitial Nephritis
- Kidney Cancer
- Polycystic Kidney Disease
- Hemolytic Uremic Syndrome
- Renal Artery Stenosis
- Nephrotic Syndrome
- End-Stage Kidney Disease
- Kidney Failure, both Acute and Chronic
A Nephrologist can also be involved when other factors cause kidney disease or dysfunction, including:
- High Blood Pressure
- Diabetes
- Heart Disease
- Autoimmune Conditions, such as Lupus
- Medications
Summary of Services
TESTS AND PROCEDURES A NEPHROLOGIST MIGHT PERFORM OR ORDER
If you’re visiting a nephrologist, they may be involved in performing a variety of tests and procedures or interpreting the results.
Laboratory Tests
A wide range of tests can be used to assess the function of your kidneys. These tests are typically performed using either a blood or urine sample.
Blood Tests
- Glomerular filtration rate (GFR). This test measures how well your kidneys are filtering your blood. GFR begins to decrease below normal levels in kidney disease.
- Serum creatinine. Creatinine is a waste product and is present at higher levels in the blood of people with kidney dysfunction.
-
Blood urea nitrogen (BUN). As with creatinine, finding high levels of this waste product in the blood is a sign of kidney dysfunction.
Urine Tests
- Urinalysis. This urine sample can be tested with a dipstick for pH as well as the presence of abnormal amounts of blood, glucose, protein, or bacteria.
- Albumin/creatinine ratio (ACR). This urine test measures the amount of protein in your urine. Albumin in the urine is a sign of kidney dysfunction.
- 24-hour urine collection. This method uses a special container to collect all of the urine that you produce during a 24-hour period. Further testing can be performed on this sample.
- Creatinine clearance. This is a measure of creatinine from both a blood sample and a 24-hour urine sample that’s used to calculate the amount of creatinine that’s exited the blood and moved to the urine.
Procedures
In addition to reviewing and interpreting the results of your laboratory tests, a Nephrologist may also perform or work with other specialists on the following procedures:
- Imaging Tests of the Kidneys, such as Ultrasounds, CT Scans, or X-Rays
- Dialysis, Including Placement of the Dialysis Catheter
- Kidney Biopsies
- Kidney Transplants
When to see a nephrologist?
Your primary care doctor can help prevent and treat the early stages of kidney disease. However, these early stages may have nonspecific symptoms such as fatigue, sleep problems and changes in the amount you urinate or in some cases, no symptoms at all.
Regular testing can monitor your kidney function, particularly if you’re at risk for kidney disease. These groups include people with:
- High Blood Pressure
- Diabetes
- Heart Disease
- A Family History of Kidney Problems

Testing can detect signs of decreasing kidney function, such as a decreasing GFR value or an increase in the level of albumin in your urine. If your test results indicate rapid or continuing deterioration of kidney function, your doctor may refer you to a Nephrologist.
Your doctor may also refer you to a nephrologist if you have any of the following:
- Advanced chronic kidney disease
- Large amounts of blood or protein in your urine
- Recurring kidney stones, though you may also be referred to a Urologist
- High blood pressure that continues to be high even after taking Medication
- A rare or inherit cause of kidney disease
Common Conditions
Chronic kidney disease (CKD) indicates that the kidneys are not working as well as they should because some of the nephrons have become damaged. The kidneys are less able to filter off the waste products. Wastes can build to high levels in your blood and make you feel sick.
You may develop complications like high blood pressure, anemia (low blood count), weak bones, poor nutritional health, and nerve damage. Kidney disease may increase your risk of having heart and blood vessel disease.
These problems may occur slowly over a long period of time. In the early stages, you may not feel sick. Your family doctor may only find an abnormal lab or protein in your urine. Early detection and treatment are important to keep your kidneys as healthy as possible – for as long as possible. Although there are many causes of CKD, high blood pressure and diabetes are the two main causes in the United States.
Polycystic kidney is a very common genetic problem (1 in 400 to 1 in 1000 people) leading to the development of large kidneys, which are enlarged by the presence of cysts. These cysts can also develop in other organs, such as the liver and the pancreas. There is a variable expression of the problem within families, and not everybody with polycystic kidney disease will develop kidney failure – maybe 50-75% will progress. The genes responsible for this disease have been found. Often polycystic kidney disease will not cause anemia, as the kidneys still produce erythropoietin. Polycystic kidney disease can cause pain, urinary infections, and blood in the urine.
It is not unusual for people with chronic kidney failure to have low levels of Vitamin D. Your doctor may check your Vitamin D level and if it is low, order a supplement. The amount prescribed to rebuild Vitamin D levels may sound like an enormous amount — a typical dose is 50,000 IU ergocalciferol (Vitamin D2) once a week for 6 to 12 weeks. Very large doses such as this are needed to rebuild stores of Vitamin D when there is a deficiency. Healthy kidneys are rich with Vitamin D receptors and play a major role in turning Vitamin D into its active form, 1,25-dihydroxyvitamin D or calciferol. When Vitamin D is in its active form, it helps balance calcium and phosphorus in your body by controlling absorption of calcium and phosphorus from the food you eat and regulates parathyroid hormone (PTH). When kidneys fail, their ability to activate Vitamin D is lost. Without the activated Vitamin D to control calcium and phosphorus levels in the blood, parathyroid hormone (PTH) will try to over compensate and go out of range.
Glomerulonephritis can develop in an acute (sudden, rapid onset) or a chronic (slow) form, and is caused by a painless inflammation of the glomerulus (the kidney filter). It can occur by itself or as part of a more general problem such as systemic lupus erythematosus (SLE). Testing of the urine shows the presence of blood and protein. It is associated with high blood pressure and progressive decline of kidney function. It is diagnosed by blood tests and a kidney biopsy. High blood pressure and the presence of protein in the urine may predict the tendency towards progression. Many patients with glomerulonephritis will simply need to be followed-up each year in an outpatient setting. Others may need treatment with specific drugs to reduce inflammation, such as steroids, azathioprine, cyclosporin A, and cyclophosphamide.
INCLUDE IMAGE
Edema is swelling caused by excess fluid trapped in the body’s tissues (fluid retention). Edema may be generalized or local. Swelling caused by edema commonly occurs in the hands, arms, ankles, legs and feet. It can appear suddenly, but usually develops subtly. You may first gain weight, or wake up with puffy eyes.
Damage to the kidneys can cause decreased levels of protein in your blood. This can contribute to capillary leaking and swelling. The edema associated with kidney disease usually occurs in your legs and around your eyes. Often, patients wait until symptoms are well advanced before seeking medical help.
A narrowing of the kidney blood vessels will lead to the kidney being starved of a good enough blood supply. This leads to the kidney becoming smaller. Often it presents with high blood pressure. If this problem exists in both kidneys, it can lead to kidney failure and pulmonary edema (fluid in the lungs causing breathlessness).
The problem may be suggested by a kidney ultrasonogram which shows one kidney is smaller than the other, but can only be diagnosed with certainty by an angiogram of the kidney blood vessels.
Sometimes it may be felt that the narrowing should be stretched open using a fine, narrow balloon (angioplasty) and then kept open with a tube inserted into the blood vessel (a stent). All of this can be done from the “inside,” during a procedure similar to an angiogram. For anyone with this disorder, the blood pressure will be controlled, the cholesterol level checked and normalized, and aspirin may be given.
Glomerulosclerosis is a general term to describe scarring of the kidneys’ tiny blood vessels, the glomeruli, which are the functional units in the kidney that filter urine from the blood. This disease may result in proteinuria (abnormal amounts of protein in urine). A kidney biopsy (removal of tiny part of kidney with a needle) may be necessary to determine whether a patient has glomerulosclerosis, or another kidney problem. Scarred glomeruli cannot be repaired, and many patients with glomerulosclerosis get worse over time until their kidneys fail. This condition is called end-stage renal disease (ESRD), and patients must undergo dialysis treatment or a kidney transplant.
The #1 cause of kidney failure is diabetes. Kidney damage develops in about 20% of patients with both type 1 and type 2 diabetes. Problems start after 10 to 15 years of diabetes, and the kidney problems are associated with diabetic eye disease. Poor control of blood glucose and high blood pressure are factors which lead to this problem, and make it worse once it starts. Recent work has shown that lowering blood pressure, particularly using ACE inhibitors at the earliest stages, can have a major impact on reducing the progression of kidney disease.
Kidney stones are one of the most common disorders of the urinary tract.
High concentrations of natural chemicals in the urine can lead to crystal formation. Under special circumstances, these small crystals may “clump” together to form a kidney stone. The majority of kidney stones create no symptoms. Kidney stones vary in size, and a stone may stay in the kidney or travel down the urinary tract. A small stone may pass on its own, causing little or no pain. A larger stone may get stuck along the urinary tract and block the flow of urine – causing symptoms that include back pain, lower abdominal pain, urinary tract infection or blood in the urine.
It is estimated that 60-80% of people with a kidney stone will form another stone within 10 years of the first episode. Removal of an existing stone does not prevent further stone formation. Medication, changes in diet and lifestyle modification may prevent kidney stone formation. A Nephrologist can help you determine the treatment to prevent new stone formation, while a Urologist can remove existing stones if needed.
Hematuria is defined as the presence of red blood cells in the urine. It can be characterized as either “gross” (visible to the naked eye) or “microscopic” (visible only under the microscope). Microscopic hematuria is an incidental finding often discovered on urine tests as part of a routine medical evaluation, whereas gross hematuria could prompt you to visit the doctor. Hematuria can originate from any site along the urinary tract, including the kidneys, ureters, bladder, prostate and urethra.
Lupus, or systemic lupus erythematosus (SLE), is an inflammatory disease resulting from an abnormality in the body’s immune system regulation. It is an unpredictable disease, varying a great deal from one case to another. A potentially serious disorder, systemic lupus erythematosus affects women much more often than men. In about eighty percent of SLE cases, joint inflammation occurs. The inflammation may affect connective tissues throughout the body and cause problems in one or more of the body’s organs, including the eyes, muscles, heart, lungs, and kidneys. In some people, systemic lupus erythematosus can produce potentially life-threatening complications, including kidney failure.
Nephrotic syndrome is not a single underlying disease, but develops alongside other processes such as glomerulonephritis or diabetes. The kidneys pass large amounts of protein (the urine may be “frothy”) into the urine and this means the water in the blood stream passes into the tissues, particularly the feet and around the eyes. Usually, it is caused by glomerulonephritis such as minimal change nephropathy (the most common in children) or membranous glomerulonephritis.
The kidney function may be absolutely normal and the only problem is the protein leak. Treatment includes restricting the fluid intake, using diuretics and perhaps aspirin and cholesterol-lowering drugs. A kidney biopsy will be done to determine the exact nature of the problem and to decide if treatment with steroids or other drugs is needed.
Renal bone disease (also known as renal osteodystrophy) is due to changes in mineral metabolism and bone structure, and occurs to some degree in everyone with progressive renal disease. Renal bone disease can be slowed or perhaps even prevented with early intervention using dietary measures and medications such as phosphate binders and calcitriol. Recently, new phosphate binders and a new class of drugs, the calcimimetics, have been introduced. Sometimes surgery (parathyroidectomy) is needed.
